Dr Stephen John Middleton MA MD FRCP FAHE
Consultant Gastroenterologist

Current Clinical Practice

Dr Stephen Middleton was appointed as a consultant gastroenterologist at Addenbrooke's hospital Cambridge in 1995 and became the senior consultant in the department from 2003. His regular practice included outpatient clinics, where he consulted patients with conditions such as IBS, Colitis, Crohn's and indigestion. He has 30 years experience in conducting colonoscopy, therapeutic endoscopy and inpatient Gastroenterology. He founded the Gastroenterology physiology unit in 1997 which provides a regional service for oesophageal manometry and ambulatory pH studies to investigate swallowing problems and indigestion. He has now retired from clinical practice to focus on medico-legal work.
Dr Middleton has been the clinical lead of the Cambridge service for irritable bowel syndrome. He was instrumental in establishing the use of dietary manipulation as the primary mode of treatment. An audit of 1000 patients revealed that dietary treatment was successful in over 70% of patients.
He established two teams of consultants who meet regularly to discuss patients with indigestion and swallowing problems (The upper GI multidisciplinary team) and patients with constipation and evacuatory disorders (lower GI multidisciplinary team). Both teams have now expanded and developed, have been running for over 2 decades and offer a wide range of diagnostic and therapeutic expertise and provide a region wide service as well as having a national referral base. Having been the local medical adviser for the National Association of Crohn’s and Colitis, (NACC) Dr Middleton has much experience in the management of patients with inflammatory bowel disease. He has a particular interest in the dietary treatment of Crohn's disease. Much of his research has been in this field and he was the UK Chief Investigator for a large Global study concerning the use of Infliximab treatment (a monoclonal antibody against a chemical called TNF that promotes Crohn’s disease) and the UK lead for the global registry of patients with ulcerative colitis. He has contributed to the research field of inflammatory bowel diseases and published on the subject in medical journals such as The Lancet, New England Medical Journal, GUT and Gastroenterology.
Dr Middleton has a strong interest in nutrition and small intestinal failure, and had a lead role in the development of the UK small intestinal transplantation programme. The first procedure was undertaken in Cambridge in 1991 and he has been involved in the programme since this time. He co- founded the National Adult Small Intestinal Transplantation Forum (NASIT forum) and was co-chair for this forum which is the national meeting for discussing and listing patients for transplantation. Medical student teaching is an integral part of the practice of a teaching hospital consultant. Dr Middleton was the lead clinician for the Cambridge University Hospital Gastroenterology clinical teaching programme for over 10 years, and has also given regular pre-clinical lectures over this period, lectures nationally and internationally including delivering a Friday Evening Discourse, in the Faraday lecture theatre, at the Royal Institute, London.
Training and Posts
Medical training in London (St Bartholomew’s hospital) 1979- 1984 Medical pre-registration house Job - Professorial unit St. Bartholomew’s hospital. Registrar posts : St Mary’s Hospital London Cambridge University Teaching hospital Addenbrooke’s. 1990 - 1993 Senior Registrar Cambridge University Teaching hospital Addenbrooke’s: 1993 – 1995. Consultant Gastroenterologist and physician Cambridge University, Addenbrooke’s hospital 1995 - 2023. Clinical lecturer University of Cambridge -1999 Senior Research Fellow, University of Cambridge – 2007. Honorary Consultant Gastroenterologist – St Mark’s hospital and academic institute, Northwick park, Harrow, London - 2007 Honorary Professor of Gastroenterology, Peninsula medical school, Devon – 2014
Research and Education
As part of his contribution to the field of Gastroenterology, Dr Middleton has been active in research since 1990 when he was appointed as the Cambridge Gastroenterology research fellow. Over the intervening period he has published over 75 peer reviewed articles including papers in prestigious medical journals such as New England medical Journal, Lancet, Gastroenterology, British Journal of Gastroenterology (GUT), Transplantation and The American Journal of Gastroenterology.
He has been active as an educationalist making multiple contributions to the “Oxford Text Book of Medicine”, “The Medicine series” and many other book chapters. He was the lead for Cambridge medical student training for over a decade and examiner for Cambridge medical finals, as well as PhD examiner for the MRC. He has delivered numerous national and international lectures including a Friday evening discourse at the Royal Institution with the former director, Sir John Meurig Thomas.
Dr Middleton had an active research programme since 1990, training many registrar grade gastroenterologists and has largely focused on the treatment of Inflammatory Bowel Disease (Crohn’s and Colitis), the Irritable Bowel Syndrome, functional bowel disorders and intestinal transplantation. He discovered that nitric oxide was an important part of the pathogenesis of Ulcerative colitis.
His has been the Chief investigator for several national and international studies and post marketing registries for the treatment of ulcerative colitis, Crohn’s disease, and the irritable bowel syndrome. He has used and developed dietary treatments and Cambridge is widely recognised as a leading centre for these treatments. The mechanism by which these treatments work has long been a mystery but the recent identification of genes linked to Crohn’s disease, also undertaken in Cambridge have now thrown light on this area and suggest the benefit of the diet may be through its effect on the intestinal bacteria.
Dr Middleton has undertaken research into the cause and treatment for the irritable bowel syndrome (IBS) which has predominantly focused on the dietary treatment of the condition. The Cambridge exclusion diets have long been successful treatments for IBS and avoid the need for drug therapy. The dietary approach to treating IBS is now very well established and has become national and international practice.
He also discovered how the muscle tone of the large intestine is modulated and controlled which explains the cause of several disorders of the intestine.
Over the last decade Dr Middleton has been working on a new syndrome which is caused by a fall in blood sugar levels after eating, often associated by bloating, chronic fatigue, cognitive impairment and nausea, which in some cases is preceded by diarrhoea. He has determined that this is caused by rapid gastric emptying and as he was the first person to identify the syndrome it has be named “Middleton Syndrome”.
Peer reviewed reseach papers
Peer Reviewed Publications 1: Percutaneous balloon valve dilatation (1989). S J Middleton British Medical Journal 6; 298(6682): 1251
2: Haemorrhagic pancreatitis: A cause of death in severe potassium permanganate poisoning. S J Middleton, M Jacyna, R Robinson and H C Thomas. Postgrad Med J 1990; 66: 657-658
3: Endoscopic and histological findings in subjects with and without dyspepsia. (1991). S J Middleton, J O Hunter. British Medical Journal 302: 1083.
4: Impending paradoxical embolism, a rare but important diagnosis c M E Speechly-Dic, S J Middleton, R A Foale. Br Heart J 1991; 65 (3): 1163-5.
5: The role of faecal Candida albicans in the pathogenesis of food intolerant irritable bowel syndrome. S J Middleton, A Coley, J O Hunter. Postgrad Med J 1992; 68:453-454
6: 99Tcm and 111In leucocyte scintigraphy in inflammatory bowel disease. D J Li., S J Middleton, E P Wraight. Nuclear Medicine Communications 1992; 13: 867-870.
7:Relaxation of distal colonic circular smooth muscle by nitric oxide derived from human leucocytes. S J Middleton, M Shorthouse, J O Hunter. Gut 1993; 34: 814-817
8: Nitric oxide affects mammalian distal colonic circular smooth muscle by tonic neural inhibition. S J Middleton, A W Cuthbert, M Shorthouse, J O Hunter. B J Pharmacol 1993; 108: 974-979.
9: Increased nitric oxide synthesis in ulcerative colitis. S J Middleton, M Shorthouse, J O Hunter. Lancet 1993;341: 465-466
10: Therapeutic aspects of nutrition in Crohn's disease. S J Middleton, J O Hunter. Journal of the Irish Colleges of Physicians and Surgeons 1995; 24(1).
11: Nitric Oxide in Ulcerative Colitis. P D Reynolds, S J Middleton, G M Hansford, J O Hunter. Lancet 1995; 345: 448.
12: Long chain triglycerides reduce the efficacy of enteral feeds in patients with active Crohn's disease. S J Middleton, J T Rucker, G A Kirby, A M Riordan, J O Hunter. Hunter. Clinical Nutrition 1995; 14: 229-236.
13: Nitric oxide synthesis in gastric mucosa. S J Middleton, ,P D Reynolds, M Shorthouse, J O Hunter, S Moss. Gut 1995; 36(6): 942
14: Validation of 99Tcm-HMPAO leucocyte scintigraphy in ulcertive colitis by comparison with histology. S J Middleton, D Li, S Wharton, P D Reynolds, E P Wraight, J O Hunter. Br J Radiology 1995; 68: 1061-1066
15:The effects of aminosalicylic acid derivatives on nitric oxide in a cell free system. P D Reynolds, S J Middleton, M Shorthouse, J O Hunter. Alimentary Pharmacology & Therapeutics 1995; 9: 491-95
16: Increased nitric oxide synthesis in ulcerative colitis. S J Middleton, J O Hunter. Inflammatory Bowel Diseases (G N J Tytgat, J F W M Bartelsman, S J H Van Deventer, eds). Kluwer Academic Publishers, Dordrecht. pp.101-105
17: N-3 Polyunsaturated fatty acids in the treatment of inflammatory bowel disease. J O Hunter, J T Woolner, S J Middleton. Proceedings of the Falk Symposium No. 96, held in Freiburg, Germany October 30 - Nov 1 1996.
18:Confirmation of nitric oxide synthesis in active ulcerative colitis by infra-red diodelaser spectroscopy. P D Reynolds, S J Middleton, G M Hansford, J O Hunter. European Journal of Gastroenterology and Hepatology 1997; 9: 463-466.
19:Multiple frequency bioimpedance: a bed-side technique for assessment of fluid shift patterns in a patient with severe dehydration. O Dewit, L Ward, S J Middleton, C Watson, P J Friend, M Elia. Clinical Nutrition 1997; 16: 189-192
20: Intestinal transplantation between two identical triplets. R Y Calne, P J Friend, S Middleton, N V Jamieson,C J E Watson, A Soin, R Chavez-Cartaya. Lancet 1997 Oct.11;350(9084):1077-8
21:Distribution of glutaminase and glutamine synthetase activities in the human gastrointestinal tract. L A James, P G Lunn, SMiddleton, M Elia. Clinical Science 1998: 94: 313-319
22:Quantitation of DNA from Exfoliated Colonocytes isolated from Human Stool surface as a Novel Non invasive Screening test for Coloectal Cancer. A Lotkionov, I K O’Neill, K R Silvester, J Cummings, S J Middleton and R Miller. Clinical Cancer Research 1998; 4: 337-342
23:Glutamine oxidation and utilization by rat and human oesophagus and duodenum. L A James, P G Lunn, S J Middleton, M Elia. Br Journal of Nutrition 1999; 81; 323-329
24:Paroxysmal nocturnal haemoglobinuria mimicking Crohn’s disease. S Sivakumaran, J O Hunter , S Middleton. GUT 1999; 44: 889
25:Small intestine transplantation from cadaver donors: procurement procedure. R Chavez-Cartaya, NV Jamieson, PJ Friend, S Middleton, RY Calne. Transplant proc 1999; 31(6): 2565-6
26:Intestinal Transplantation: 1997 Report of the International Registry. D Grant of behalf of the Intestinal Transplant Registry.Transplantation 1999 Vol. 67, 1061-1064, No. 7
27:Treatment of oesophageal Crohn's disease by Enteral feeding via percutaneous endoscopic gastrostomy. T Thomas, E Berto, M Scribano, S J Middleton, J O Hunter. Journal of Parenteral and Enteral Nutrition 2000, Vol.24, No.3
28:Management of Acute Diarrhoea. EAB Cameron, SJ Middleton. CPD Journal Internal Medicine 2000, Vo1.1 No.3
29:Evaluation of the effectiveness of a specialist nurse in the management of inflammatory bowel disease (IBD). A Nightingale, W Middleton, SJ Middleton, JO Hunter. European Journal of Gastroenterology & Hepataology 2000, 12:1 - 7
30:Neuronal COX-2 expression in human myenteric plexus in active inflammatory bowel disease. P J Roberts, K Morgan, R Miller, JO Hunter SJ Middleton. GUT 2001; 48: 468-472
31:The physiological expression of inducible nitric oxide synthase (Inos) in the human colon. PJ Roberts, GP Riley, K Morgan R Miller, JO Hunter, SJ Middleton. Journal of Clinical Pathology 2001; 54: No 4: 293-297
32:Parenteral nutrition and small bowel transplantation as treatments for irreversible intestinal failure in adults. EAB Cameron, JAH Binnie, SJ Middleton. TTMed-Gastroenterology. August 2001.
33:A family history study of chronic fatique syndrome. G M Walsh, N Z Sainal, S J Middleton, E S Paykel. Psychiatric Genetics 2001. 11:No:3
34:3 year prospective validation of a pre-endoscopic risk stratification in patients with acu upper GI haemorrahage. EAB Cameron, JN Pratap, TJ Sims, S Inman, D Boyd, M Ward, SJ Middleton. Euro.Journal of Gastroenterology & Hepatology 2002; 14: No5. 35
35:Quality of life in adults following small bowel transplantation. EAB Cameron, JAH Binnie, Jamieson, S Pollard SJ Middleton. Transplantation Proceedings. 2002; 34, 000.
36: Rofecoxib and cytomegalovirus in acute flare up of ulcerative colitis: Co-precipitants or co incidence? J Goh, D Wight, M Parkes, SJ Middleton, JO Hunter. American Journal of Gastroenterology. 2002 Apr;97 (4):1061-2.
37:Expression of isoforms of nitric oxide synthase in collagenous colitis. EAB Cameron, S J Middleton. GUT 2002; 50(6).
38:A double blind-randomised placebo-controlled trial of essential fatty acid supplementation in maintenance of remission in ulcerative colitis. SJ Middleton, S Naylor, J Woolner, JO Hunter. Alimentary Pharmacology & Therapeutics. 2002; 16: 1131-1135.
39:Efficacy and safety of renzapride in patients with constipation-predominant irritable bowel syndrome. NL Meyers, J Tack, S Middleton, M Horne, H Piessevau
40:Irritable bowel syndrome. Stephen Middleton. Primary Health Care, 2002; 12: No10 1 December 2002.
41:The Significance of Low-Grade Uptake in Tc-99m HMPAO-WBC Imaging for Inflammatory Bowel Disease. K Balan, C Beadsmoore, A Groves, C Solanki, S Middleton, A Freeman. World Journal of Nuclear Medicine. 2003; 2:92-95.
42:Elemental diet in the treatment of orofacial Crohn’s disease. EAB Cameron, SJ Middleton. GUT. 2003; Vol.52 1:143.
43:Adult small intestinal transplantation in England and Wales. SJ Middleton, S Pollard, PJ Friend, C Watson, RY Calne, M Davies, EA Cameron, AE Gimson, JA Bradley, J Shaffer, NV Jamieson. British Journal of Surgery. 2003; 90: 723-727.
44: Oral prednisolone metasulphobenzoate in the treatment of active ulcerative colitis Predocol i n Ulcerative Colitis. EAB Cameron, JAH Binnie, K Balan, SA Skerratt, A Swift, C Solanki, SJ Middleton. Scand J Gastroenterol.2003; 5:535-537.
45:Relapsing encephalopathy following small bowel transplantation. SM Shah, PJRoberts, CJE Watson, PJ Friend, NV Jamieson, RY Calne, SJ Middleton. Transplant Proceedings. Transplantation Proceedings 35, 156-1566 (2003).
46: Small-intestinal dysfunction accompanies the complex endocrinopathy of human proprotein convertase 1 deficiency. RS Jackson, JWM Creemers, IS Farooqi, ML Rffin-Sanson, a Varro, GJ Dockray, JJ Holst, PL Brubaker, P Corvol, KS Polonsky, D Ostreta, KL Becker, Z Bertagna, JC Hutton, A White, MT Dattani, K Hussain, SJ Middleton, TM Nicole, PJ Milla, KJ Lindley and S O’Rahilly. The Journal of Clinical Investigation. 2003; Vol 112 No10.
47:Diagnosis of oesophageal cancer by detection of minichromosome maintenance 5 protein in gastric aspirates (orginal research article. GH Williams, R Swinn, AT Provost, P de Clive-Lowe, I Halsall, JJ Going, CN Hales, K Stoeber and SJ Middleton. Brtitish Journal of Cancer. (2004) 91, 714-719.
48:Quantification of disease acvtivity in patients undergoing leucocyte scintigraphy for suspected inflammatory bowel disease. Middleton SJ, Peters AM. Eur J Nucl Mol imaging. 2004 Cheow etal,
49:The current status of small intestinal transplantation in the UK and internationally. S J Middleton and N V Jamieson. 2005 Gut (54): 1650-1657
50:Pilot study of the efficacy of renzapride on gastrointestinal motility and symptoms in patients with constipation predominant IBS. 2006 J Tack, SJ Middleton, MC Horne, H Piessevauvs, JS Bloor, NL Meyers, RMJ Palmer.
51:Is intestinal transplantation now an alternative to parenteral nutrition for patients with intestinal failure ? Proc Nutr Soc. 2007 Aug;66(3):316-20. Review
52:Cambridge-Miami score for properative risk assessment : initial developmnt and validation Middleton, Nishida, Tzakis, Woodward, Duncan, Watson, Wiles, Sivaprakasam, Butler, Gabe, Jamieson. Transpant proceedings 2010 42(1):19-21
53:Utility of whole gut transit scintigraphy in patients with chronic gastrointestinal symptoms. Balan K, Alwis L, Sonoda LI, Pawaroo D, Parry-Jones DR, Middleton S Nucl Med Commun. 2010 Apr;31(4):328-33.
54:Clinical significance of scintigraphic rapid gastric emptying. Balan K, Sonoda LI, Seshadri N, Solanki C, Middleton S. Nucl Med Commun. 2011 Dec;32(12):1185-9.
55:Post-prandial reactive hypoglycaemia and diarrhea caused by idiopathic accelerated gastric emptying: a case report. Middleton SJ, Balan K. J Med Case Rep. 2011 May 13;5:177
56:Idiopathic accelerated gastric emptying presenting in adults with post-prandial diarrhea and reactive hypoglycemia: a case series. Middleton SJ, Balan K. J Med Case Rep. 2012 May 19;6(1):132
57: Intestinal transplantation : Review article for Medicine series – the latest developments. Medicine,2012 (39):3; 183-190
58:Case Report: Multidrug-Resistant Cytomegalovirus in a Modified Multivisceral Transplant Recipient. Petra M. Goldsmith; Mir Mubariz Husain; Andrew Carmichael; Hongyi Zhang; Stephen J.Middleton. Transplantation April 15, 2012, Volume 93, Issue 7
59:Vedolizumab as induction and maintenance therapy for Crohn's disease. GEMINI 2 Study Group. N Engl J Med. 2013 Aug 22;369(8):711-21.
60:Preoperative comorbidity correlates inversely with survival after intestinal and multivisceral transplantation in adults. Sivaprakasam R, Hidenori T, Pither C, Nishida S, Butler AJ, Island ER, Moon J, Dawwas M, Gab e SM, Jamieson NV, Tzakis AG, Middleton SJ.J Transplant. 2013;2013:202410
61:Use of the alpha glucosidase inhibitor acarbose in patients with 'Middleton syndrome': normal gastric anatomy but with accelerated gastric emptying causing postprandial reactive hypoglycemia and diarrhea. Playford RJ, Pither C, Gao R, Middleton SJ Can J Gastroenterol. 2013 Jul;27(7):403-4.
62:Panaccione R, Ghosh S, Middleton S, Márquez JR, Scott BB, Flint L, van Hoogstraten HJ, Chen AC, Zheng H, Danese S, Rutgeerts P. Combination Therapy With Infliximab and Azathioprine Is Superior to Monotherapy With Either Agent in Ulcerative Colitis.Gastroenterology. 2013 Oct 25. pii: S0016-5085(13)01526-6
63:Preoperative comorbidity correlates inversely with survival after intestinal and multivisceral transplantation in adults. Sivaprakasam R, Hidenori T, Pither C, Nishida S, Butler AJ, Island ER, Moon J, Dawwas M, Gabe SM, Jamieson NV, Tzakis AG, Middleton SJ. J Transplant. 2013;2013:202410
64:Delayed dynamic abdominal wall closure following multi-visceral transplantation. Iype S, Butler A, Jamieson N, Middleton S, Jah A. Int J Surg Case Rep. 2014;5(12):988-91. doi: 10.1016/j.ijscr.2014.08.006. Epub 2014 Oct 13.
65:Psychiatric disorders in patients undergoing intestinal transplantation. Pither C, Green J, Butler A, Chukaulim B, West S, Gao R, Gabe S, Middleton SJ. Transplant Proc. 2014 Jul-Aug;46(6):2136-9.
66: Prothrombotic disorders in a cohort of 25 patients undergoing transplantation: investigation and management implications. Pither C, Middleton S, Gao R, Sharkey L, Jamieson N, Butler A. Transplant Proc. 2014 Jul-Aug;46(6):2133-5.
67:Adult small intestinal and multivisceral transplantation: lessons through the "retrospecto-scope" at a single UK centre from 1991 to 2013. Middleton SJ, Pither C, Gao R, Duncan S, Green J, Sharkey L, Chukualim B, Kratzing C, Woodward J, Gabe SM, Jamieson N, Butler A. Transplant Proc. 2014 Jul-Aug;46(6):2109-13
68:Quality of life and performance status before and after small intestinal transplantation. Pither C, Duncan S, Gao R, Butler A, West S, Gabe SM, Middleton SJ. Transplant Proc. 2014 Jul-Aug;46(6):2114-8
69: Occult invasive aspergillosis infection following multivisceral transplantation.Rutter CS, Sharkey LM, Gao R, Pither C, Ibrahim A, Enoch DA, Butler AJ, Middleton SJ. IDCases. 2014 Jul 10;1(3):53-4.
70:Urgent Multivisceral Transplantation for Widespread Splanchnic Ischemia. Sharkey LM, Russell NK, Rutter CS, Middleton SJ, Bradley JA, Jamieson NV, Butler AJ. J Am Coll Surg. 2016 May;222(5):760-5.
71:Adult Intestinal and Multivisceral Transplantation: Experience From a Single Center in the United Kingdom. Rutter CS, Amin I, Russell NK, Sharkey LM, Butler AJ, Middleton SJ. Transplant Proc. 2016 Mar;48(2):468-72.
72:Stomal Cytomegalovirus Infection Following Intestinal Transplant. Ambrose T, Sharkey L,Louis-Auguste J, Butler A, Massey D, Russell N, Pursglove S, Middleton SJ. Am J Gastroenterol. 2015 Nov;110(11):1534.
73:Cytomegalovirus Infection and Rates of Antiviral Resistance Following Intestinal and Multivisceral Transplantation. Ambrose T, Sharkey LM, Louis-Auguste J, Rutter CS, Duncan S, English S, Gkrania- Klotsas E, Carmichael A, Woodward JM, Russell N, Massey D, Butler A, Middleton S. Transplant Proc. 2016 Mar;48(2):492-6.
74: Fatal breakthrough mucormycosis in a multivisceral transplant patient receiving micafungin: Case report and literature review.Louis-Auguste JR, Micallef C, Ambrose T, Upponi S, Butler AJ, Massey D, Middleton SJ, Russell N, Rutter CS, Sharkey LM, Woodward J, Gkrania-Klotsas E, Enoch DA.IDCases. 2018 Mar 24;12:76-79.
75: Graft versus host disease after multivisceral transplantation: A UK center experience and update on management.Sharkey LM, Peacock S, Russell NK, Middleton SJ, Butler AJ.Clin Transplant. 2018 May;32(5)
76: Characterisation of proguanylin expressing cells in the intestine - evidence for constitutive luminal secretion. Dye FS, Larraufie P, Kay R, Darwish T, Rievaj J, Goldspink DA, Meek CL, Middleton SJ, Hardwick RH, Roberts GP, Percival-Alwyn JL, Vaughan T, Ferraro F, Challis BG, O'Rahilly S, Groves M, Gribble FM, Reimann F. Sci Rep. 2019 Oct 30;9(1):15574.
77: Transplant-associated thrombotic microangiopathy and immune haematological complications following intestine-containing organ transplantation: experience from over 100 consecutive cases. Thomas W, Foukaneli T, Cosgrove J, Massey D, Woodward J, Middleton S, Besser M, Russell N, Amin I, Butler A, Sharkey L.Br J Haematol. 2021 Jun;193(5):961-970.

Designed by William Etheridge, and built by James Essex in 1749, it has been rebuilt on two occasions, in 1866 and in 1905, but has kept the same overall design. Although it appears to be an arch, it is composed entirely of straight timbers in a sophisticated engineering design, hence the name.
The original "mathematical bridge" had the same design, crossed the Cam between Trinity and Trinity Hall colleges and was also commissioned by James Essex.
Private Practice

Dr Middleton previously conducted private consultations and endoscopy at Nuffield hospital and Spire Cambridge Lea hospitals in Cambridge since 1996, but has now retired from this practice.
His private practice included all services he has offered during his NHS practice with the exception of intestinal transplantation which is only offered through the NHS. In addition to clinic consultations he also had inpatients and undertook colonoscopy, gastroscopy, enteroscopy and gastro-intestinal physiology including 24 hour ambulatory pH and impedance studies and high resolution manometry. He also offered a variety of advanced special investigations and services. He was particularly interested in Functional bowel disorders and is working on new dietary strategies to treat IBS.
He introduced a new wireless method (BRAVO) for detecting and measuring acid reflux (heartburn). This avoids the need for a nasal catheter and allows 2 days or more of recording whilst patients can undertake their normal activities.
Dr Middleton has also introduced a new non-invasive method for measuring the function of the entire gastrointestinal tract using a small highly sophisticated pill sized capsule (SMART PILL) which is swallowed and transmits information about the function of the stomach, small and large intestine by wireless connection to an external receiver carried by the patient to give an accurate assessment of the function of the digestive system. This can detect conditions such as gastroparesis, idiopathic accelerated gastric emptying (Middleton syndrome), and slow transit constipation. He offered a full range of special investigations such as Hydrogen and Urea breath tests, anorectal physiology and Biofeedback. These can detect small intestinal bacterial overgrowth, Helicobacter pylori infection and colonic evacuatory disorders and anal sphincter damage, respectively.
Dr Middleton has now stopped all clinical practice to concentrate on medico-legal work.
Special Interests
Click on the topic to reveal
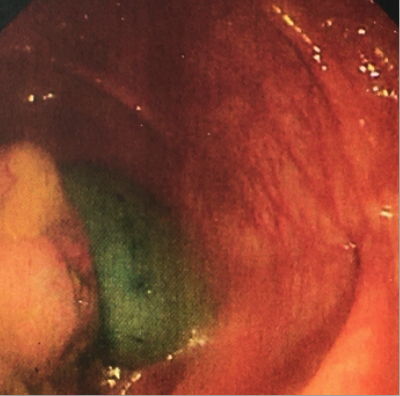
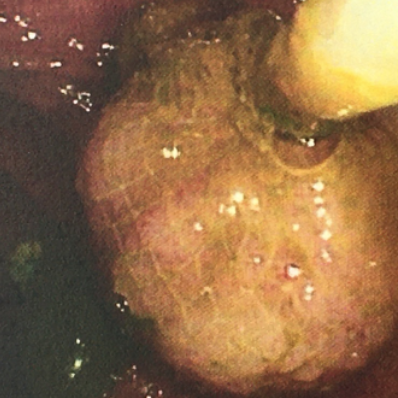
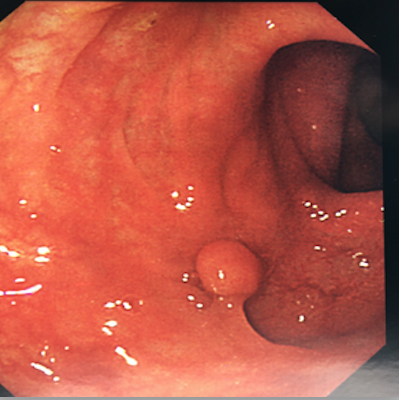
Endoscopes are flexible tubes that transmit images of the gastrointestinal tract. They vary from about 7mm to 11mm in diameter and can be steered through the stomach and bowel to allow examination and procedures such as a biopsy (taking a tiny piece of the lining for microscopic examination) removing polyps (small growths that can sometimes develop in to cancer) or dilating narrowed segments (strictures) which can cause a blockage.
Dr Middleton has been the lead gastroenterologist in Cambridge for selected endoscopic oesophageal procedures including the treatment of swallowing disorders such as Achalasia, diffuse oesophageal spasm and Nutcracker oesophagus.
He introduced the use of endoscopic Botox in Cambridge for these conditions. Before Botox there were few available treatments for these conditions and this now offers an excellent and low risk treatment. He also developed the service in Cambridge by introducing the practice of balloon dilatation to widen strictures (narrowing) of the oesophagus. These can be caused by acid reflux (heartburn) and sometimes by tumours. Since the introduction of balloon dilatation rather than bougies (rods) there have been far fewer complications of the procedure such as perforations (a split of the gullet) estimated by an early national audit to be 100 fold lower than the national average. At the same time he introduced the use of laser therapy and a new type of stent to open the narrowing caused by tumours in the oesophagus, which is made of and expandable wire (alloy mesh which has memory for shape) and much less traumatic than the former more rigid plastic stents which tended to tear the oesophagus. These techniques are now widely adopted.
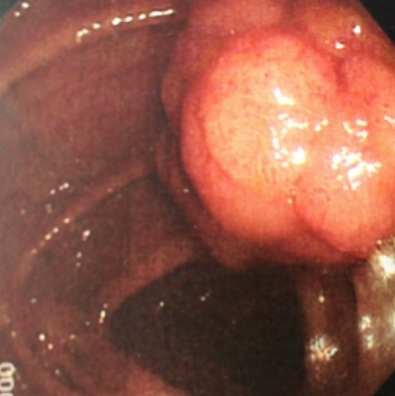

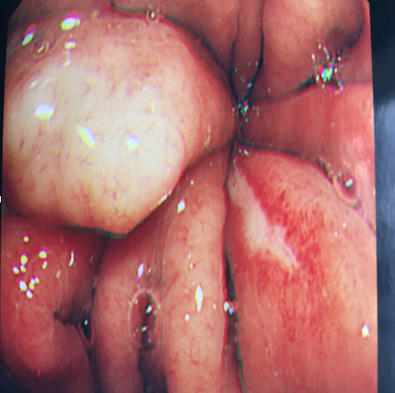
the wire loop is tightened so that it cuts through the base of the polyp. At the same time the area is cauterized by the hot wire to reduce bleeding from the polyp stump.
Dr Middleton has treated patients with IBS for over 30 years and has been the lead clinician of the IBS service in Cambridge. He has a special interest in the dietary treatment of IBS which avoids the need for drug treatments in most cases and is currently working on the development of diets that are tailored to the microbiome of individual patients.
These common and very troubling conditions often require considerable expertise when they are present in their severe forms. They can be combined with IBS which makes their treatment even more difficult. Dr Middleton and his colorectal surgical colleague established a new service for these conditions. The service pioneered the use of Biofeedback or Bowel retraining in Cambridge which is particularly effective for evacuatory disorders. These techniques have become widely adopted in specialised medical centres and are the treatment of choice for most forms of evacuatory disorder and incontinence.
Dr Middleton has had a long standing interest in nutrition and intravenous feeding having formerly been the lead clinician of the nutrition service in Cambridge. This has led him on to become one of the founders of intestinal transplantation in Cambridge in the 1990’s since when Cambridge has maintained a leading position in the national programme for adults and a prominent position in the internationally. Cambridge were the first in the UK and one of the first in the world to undertake this procedure and is recognised as one of the largest and most successful units in the world. Dr Middleton also founded the NASIT forum (National Adult Small Intestinal Transplantation forum) with a colleague from St Mark’s hospital London. This forum has been endorsed by the department of health as the official listing meeting for intestinal transplantation patients and provides a central point of contact for all those undertaking the procedure on adults in the UK where all potential patients are discussed.
Dr Middleton has over 30 years experience in treating patients with Crohn’s disease and ulcerative colitis. As well as gaining considerable experience in the use of existing treatments he has been involved in the development of new treatments for these conditions including dietary treatments and mono-clonal antibody therapies. Dr Middleton has also undertaken and supervised laboratory based studies into these conditions to better understand their scientific basis and has been the chief investigator in several large multi-national studies.
Click on the topic to reveal
• Testing and treating Helicobacter pylori infection
• Investigation and treatment of anaemia
• Investigation and treatment of nausea
• Investigation and treatment of abdominal pain
• General gastroenterology
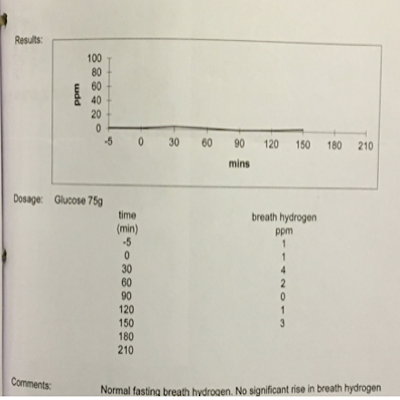
- Glucose hydrogen breath tests (to test for bacterial overgrowth of the small intestine (SIBO))
- Lactose hydrogen breath tests (to test for lactose intolerance)
- Urea breath tests (for H pylori infection)
- Oesophageal pH impedance testing (for gastro-oesophageal reflux)
- Oesophageal manometry (for chest pain and swallowing disorders)
- SMART Pill, Wireless capsule motility study (to assess the function of the stomach, small intestine and colon by swallowing a small pill size capsule)
• Gastric emptying studies (To measure the movement of food through the stomach).

It takes its name from the Bridge of Sighs in Venice, although they have little in common apart from the fact that they are both covered. The bridge is said to have been Queen Victoria’s favourite part of the city.
Conditions
Inflammatory Bowel Disease (IBD)
Inflammatory Bowel Disease (IBD) is a term referring to several inflammatory conditions of the large and small intestines which are chronic (long lasting) and leave long lasting changes to the lining of the intestines. The cause of these conditions is unknown but there are many theories. It appears that there is not a single cause but many different factors that can lead to the intestine becoming inflamed (irritated). Some of these are determined by genes of which there are many, and slight differences in the structure and function of these genes can increase the chances of developing IBD. There are also believed to be environmental factors such as bacteria, foods, stress and smoking for instance which can also influence the chance of getting these conditions.
IBD can be roughly divided into three main conditions; 1: Ulcerative colitis 2: Crohn's disease 3: Indeterminate colitis. Ulcerative colitis (UC) affects the large intestine, usually just the lining (mucosa) and can involve all or just part of the large intestine (colon) but always starts in the lower reaches (rectum) and works its way up in a continuous stretch if inflammation. Crohn's disease (CD) can affect any part of the gastrointestinal tract from the mouth to the anus and is usually patchy. It can involve deeper layers than UC.
Indeterminate colitis is somewhere in between the above two, but is usually reserved for inflammation of the large bowel which is not quite typical of UC and has some features of Crohn's disease but not enough to be sure.
The treatment of inflammatory bowel disease can be divided into two stages:
Inducing disease remission.
Maintaining disease remission.
The types of treatment available range from dietary modification to very potent immunosuppression, some of these are aimed at inducing disease remission others at maintaining remission. Several treatments achieve both these aims.

Irritible Bowel Syndrome (IBS)
Dr Middleton has treated patients with IBS for over 30 years and has been the lead clinician of the IBS service in Cambridge. He has a special interest in the dietary treatment of IBS which avoids the need for drug treatments in most cases. IBS is a common condition and reported to affect up to 40% of the UK population at some time or another. It can affect adults at any age but most often affects those in the working years and tends to develop when people are under stress. However, there are several other causes of IBS such as gastrointestinal infections like food poisoning. Although the infection resolves patients are left with an altered bowel habit, often alternating diarrhoea and constipation associated with a bloated feeling, flatulence and diffuse abdominal discomfort or pain. IBS can also cause heartburn in some cases. The cause of IBS is thought to be oversensitivity the gastrointestinal tract
The large intestine is often the source of IBS symptoms as this is the storage vessel for waste products that can irritate and produce symptoms. When the large intestine is irritated it often expels the contents which causes diarrhoea, after this it might try to hold on to it and become constipated. Any gas in the bowel is felt as discomfort or pain as the bowel is oversensitive.
IBS is never the cause of life threatening intestinal disease but its symptoms tend to overlap with those of a more serious nature, so often investigations are required to exclude these conditions which require a different sort of treatment. Your doctor will be able to advise you if this is necessary.
Treatment of IBS is very effective if a cause can be found, such as a particular source of stress, it might be possible to remove this. Often, however, it is either not possible to identify a particular cause or not feasible to remove the source. It is then necessary to start a treatment. In most cases dietary treatment seems to be preferable and this is certainly Dr Middleton’s opinion. Careful application of dietary change can result in excellent improvements in symptoms ( see treatment section) and in many cases most of the foods can be put back in to the diet. This process of dietary change has to be tailored to the individual patient, and a careful check of the final diet should be undertaken to make sure that it remains healthy for long term use. In most cases it is not a radical change, and can gradually be expanded. It is important to note that Irritable bowel syndrome is often aggravated by food intolerance but this is not the same as food allergy. This is often associated with a rash and swelling of the lips and tongue, it is a different condition and can be more serious than food intolerance and should be dealt with by your doctor and an allergy consultant.






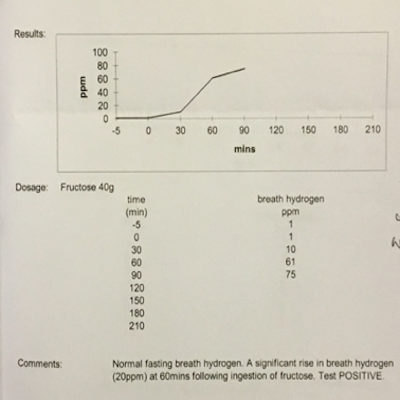
Dr Middleton uses the Dietary approach to treat IBS
How does dietary intervention improve IBS ? The underlying problem in irritable bowel syndrome is over sensitivity of the gut (hypersensitivity) and it can affect any part of the gastrointestinal tract but usually most of the symptoms arise from the large intestine. Most foods are not completely digested by the stomach and small intestine and therefore some residue enters the large bowel where the majority of bacteria reside and break down the food. We call this process fermentation. This produces side products and it is these chemicals that are believed to cause symptoms in patients with irritable bowel syndrome. Some patients report specific food intolerances. Studies have been done to try and test these scientifically, but it has proven very difficult to get consistent results. There are however a number of conditions that are caused or provoked by specific food intolerances and are well substantiated such as Lactose intolerance which is an intolerance to milk sugar. People with this condition lack the enzyme (lactase) required to digest the sugar lactose (lactase) which is usually present in the small intestine. If they ingest lactose it cannot be digested and passes into the large bowel where it is fermented by bacteria. This causes production of large amounts of gas and by-products which produce diarrhoea and bloating, similar to those experienced by those with irritable bowel syndrome. Dr Middleton usually advises dietary manipulation as the first line treatment for irritable bowel syndrome. An exclusion diet is used, there are various types of diet depending upon the symptoms experienced. Initially the diet is relatively strict, once symptoms are under control, foods can be reintroduced to establish which foods tend to provoke symptoms. Often, by avoiding a small number of foods, the symptoms can be controlled without unduly restricting the diet. Where there seem to be many food intolerances it is not wise to use the dietary strategy as this may lead to an inadequate diet that is unhealthy. Even if the dietary restrictions seem minor it is often important to have a long term diet assessed by a professional Dietitian to ensure any ongoing dietary restriction will not affect health in any way.
Dr Middleton has audited his dietary treatment strategy in Cambridge, there is a very good success rate of around 70-80% and therefore most people do not need drug therapy.
Drug therapy for irritable bowel syndrome
This can be divided into:
A]Drugs that are taken when symptoms occur. As many of the symptoms are caused by spasm of the gut, anti-spasmodic drugs are used when the pain occurs such as Mebeverine, Hyoscine, Propantheline, Alverine and Peppermint oil. These drugs tend not to work if taken all the time.
B] Drugs that are taken all the time to prevent symptoms. One of the best drugs in this category is amitriptyline, taken in a low dose and built up slowly. Although it is licensed as an anti-depressive agent, in lower doses it is given for the smooth muscle relaxing effects rather than for its anti-depressive action.
Avoiding provoking factors
In addition to avoiding foods that provoke irritable bowel syndrome, factors such as stress may aggravate symptoms. Medication may be taken before a predictable stressful event such as examinations, interviews or performing in public.

Symptoms suggesting gastrointestinal disorders
The location of pain can give a clue to its cause. Chest pain can be produced by oesophageal disorders such as muscular spasm of the oesophagus and reflux of acid into the oesophagus. Also, if there is a partial obstruction of the oesophagus such as a narrowing this can cause pain. It is very important to make certain where chest pain is coming from and one of the most important causes to exclude is heart disease such as angina and heart attacks which can cause chest pain of various types. Once the heart has been excluded as the cause investigations can proceed to find other causes. Gall bladder disease can also cause chest pain but the main gastrointestinal causes are oesophageal disorders.
Patients with pain where a gastrointestinal cause is suspected usually undergo a Gastroscopy to directly visualise the oesophagus and take small specimens called biopsies from its lining as appropriate. It is also often necessary to construct some additional imaging such as an ultrasound examination of the upper abdomen to exclude conditions such as Gall stones. Some patients require more sophisticated investigations to determine if they have gastro-oesophageal reflux disorder or oesophageal muscle disorders such as oesophageal spasm. Special tests for these conditions have been developed such as high resolution manometry and 24 hour ambulatory pH studies.
Abdominal pain can be diffuse or localised, and affect upper lower or all the abdomen (tummy). Well localised pain often suggests a well localised problem in the gut such as an ulcer. More diffuse pain might suggest a condition such as irritable bowel syndrome, but the interpretation of this symptom requires consultation with a GP, who can refer on to a specialist as required.
The type of investigation chosen to determine the cause of the pain is chosen depending on the characteristics of the pain. Where a gastric cause is suspected such as a stomach ulcer a Gastroscopy is undertaken. If a lower bowel problem seems likely then a colonoscopy is arranged. Sometimes a deeper seated problem is suspected such as a pancreatic disorder and CT scanning can provide a useful overview of the abdominal and pelvic organs.
Pain at night which causes somebody to wake from their sleep is usually not IBS and suggests another cause such as inflammation in the intestine or stomach.
If the pain is related to or eased by eating it is more likely to be arising from the GI tract. Likewise if a bowel movement relieves it the pain might well be coming from the large intestine..
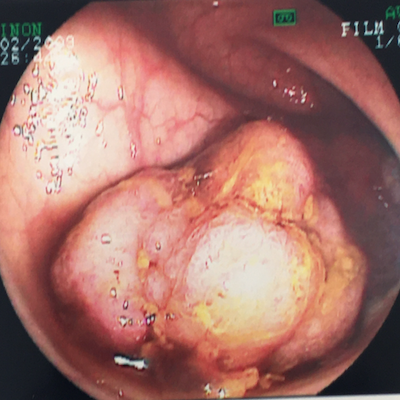
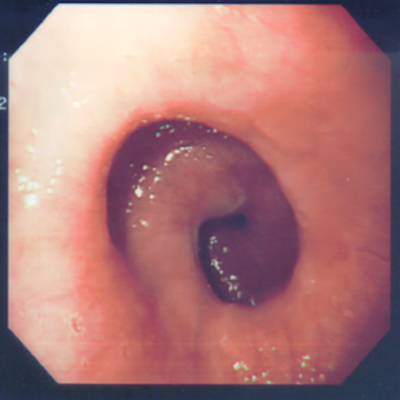
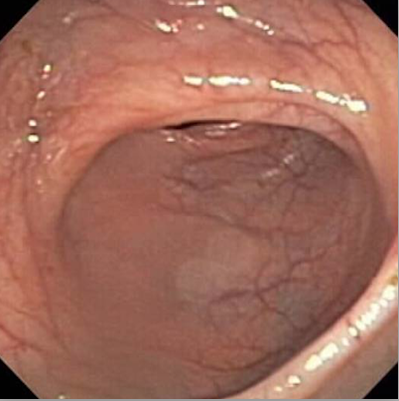
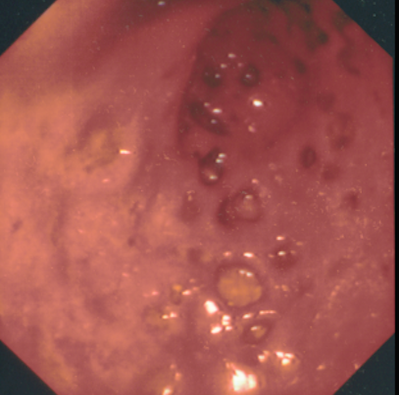
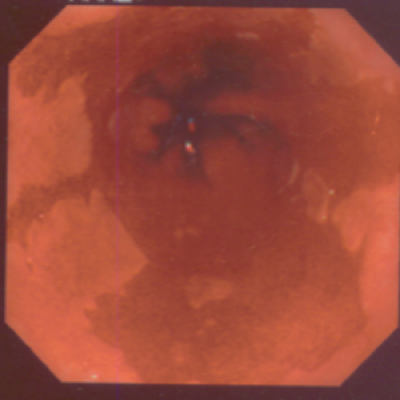
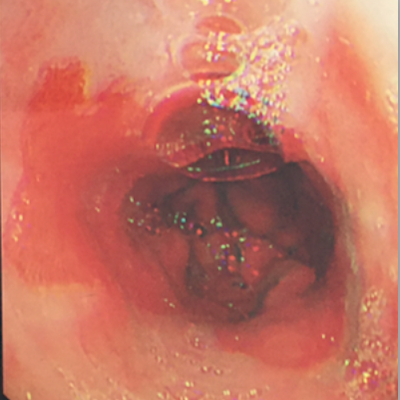
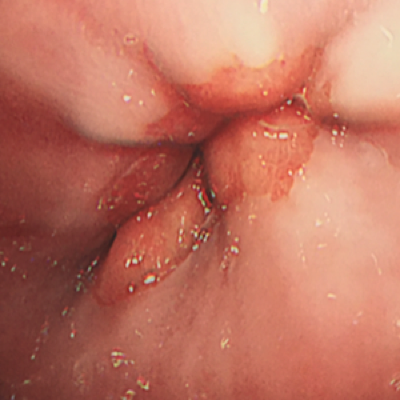
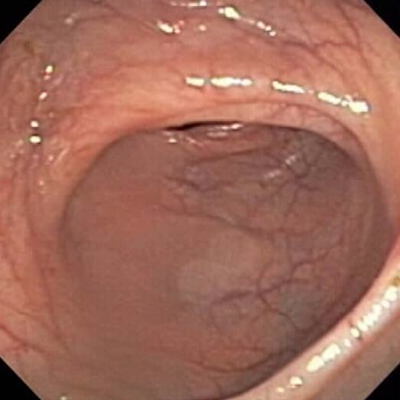
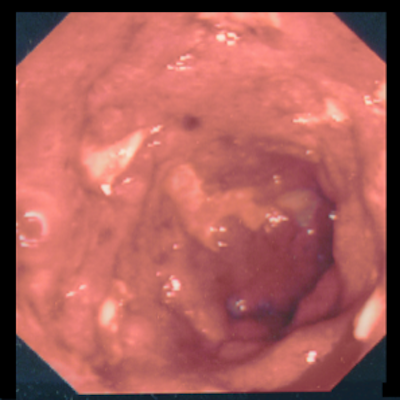
(Images taken at gastroscopy)
Heartburn The feeling of an unpleasant burning sensation behind the central rib cage in the front is described as heartburn. This is caused by fluid in the stomach coming up into the oesophagus (gullet) and irritating the oesophageal lining. The fluid usually contains acid but can also occasionally be predominantly bile. Reflux can also cause a tight feeling at the top of the throat, which sometimes gives the sensation that something is stuck in the throat (globus). Recently it has also been realised that Reflux can cause dental erosion, dissolving away the enamel of the teeth. It can also aggravate asthma and some believe it might be the cause of asthma in some patients. Some patients develop a condition called Barrett’s oesophagus (see photograph) which makes it slightly more likely to develop oesophageal cancer and these patients are screened with endoscopy depending upon how much Barrett’s they have.
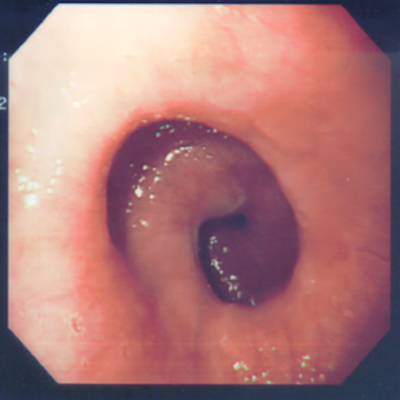
(Images taken at gastroscopy)
Diarrhoea This term is usually used to describe the passage of bowel motions (stools) which are more frequent and looser than usual. Its character can often give doctors a clue as to the cause. For instance pale stools suggest malabsorption of fat.
Inflammation of the bowel such as found in ulcerative colitis or Crohn’s disease can cause diarrhoea as can conditions that interfere with the absorption of food such as coeliac disease.
Functional bowel disorders such as IBS (irritable bowel syndrome) are perhaps the most common cause of diarrhoea.
Endoscopic examination of the bowel is usually required as this allows small specimens to be taken (biopsies) from which a definitive diagnosis can be made.
Bloating Bloating is often caused by the presence of gas. This can be produced by fermentation of food by bacteria in the intestine or by the swallowing of air. IBS is commonly associated with bloating. Upper abdominal bloating can arise due to excessive air swallowing (aerophagea)
Flatulence & Eructation The expulsion of gas in a downward (flatulence) or upward (eructation) direction is normal but if excessive can be inconvenient. Excessive eructation is often caused by air swallowing and people with Reflux often get this. Flatulence can be increased by eating certain foods and in people with lactose intolerance milk products can cause it.
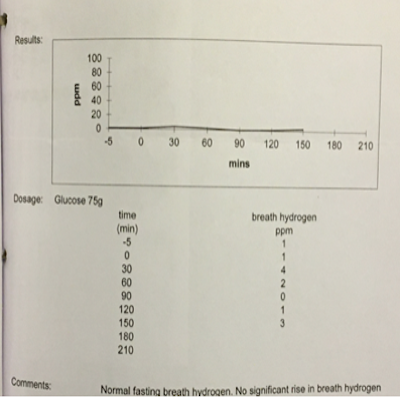
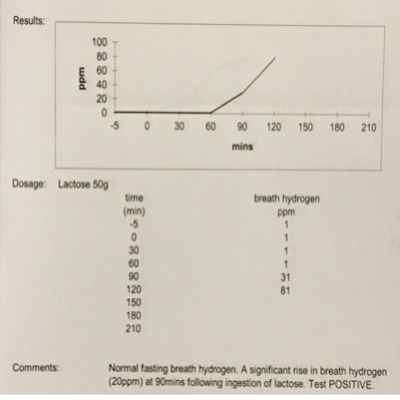
where it can be measured in the reath.
This patient had lactose intolerance.
Constipation The passage of hard stools with difficulty and discomfort or less frequently than usual is often described as constipation. Some describe constipation as the passage of less than one stool in 3 days, but it is the change in bowel habit which may indicate a problem in the bowel and when lasting longer than a few weeks should prompt individuals to seek medical advice. If there has been a definite change in bowel habit it is better to consult a doctor than use over the counter medicines as it may be possible to find the cause of the problem and sometimes these symptoms are caused by more serious conditions that require prompt treatment.
Constipation can arise from disorders that causes slowing of the transport of stools along the large bowel (slow transit constipation) or from difficulty evacuating stools at the lower end of the bowel (evacuatory disorder).
Simple constipation is very common and the cause of this may not be determined, it often occurs in conjunction with pain and bloating as a form of IBS.
Causes of slow transit constipation include metabolic causes such as thyroid disease and high serum calcium levels. But a change in diet can also cause it. More serious conditions of the large bowel often need to be excluded in older patients using colonoscopy or CT scanning. Where there are diagnostic difficulties and a muscle disorder is thought to be the cause it is also useful for selected patients to undergo transit studies such as wireless capsule motility or radionucleotide studies.
Swallowing problems When food gets stuck or feels slow going down after trying to swallow this is called dysphagia. People who experience this should always seek medical advice straight away. There are many causes and mostly they are not very serious and can be treated effectively. Occasionally, especially in older people, swallowing problems can be the sign of a more serious condition which is why medical advice should be sought at an early stage. Dysphagia may be the result of a muscle disorder of the oesophagus but can also be caused by narrowing of the oesophagus due to scarring caused by acid reflux or more rarely by cancer of the oesophagus.
This symptom is usually investigated with a prompt gastroscopy which allows direct visualisation of the oesophageal lining and for biopsies to be taken which can detect condition such as eosinophilic oesophagitis, acid reflux damage or sometimes oesophageal cancer.

Kings College Organ The Royal Saint Henry VI illustrated in the stained glass of the Chapel Henry was 19 when he laid the first stone of the 'College roial of Oure Lady and Seynt Nicholas' in Cambridge on Passion Sunday, 1441. Then the town was still a port so Henry exercised a form of compulsory purchase in the centre of medieval Cambridge, levelling houses, shops, lanes and wharves, and even a church. It took three years to purchase and clear the land. Initially King's was to have a Provost and 12 impoverished students (the number of the apostles) but after work had begun on the Old Court, Henry decided to have 70 scholars (representing the 70 early evangelists chosen by Jesus) drawn exclusively from the king's other foundation at Eton. For over 400 years King's College admitted only Etonians and claimed the privilege that its students should receive degrees without being examined. Henry drew up detailed instructions for Eton and King's, and at both places his first concern was the chapel. No other college had a chapel built on such a scale: in fact, the building was modelled on the plan of a cathedral choir, the architect being Henry VI's master mason, Reginald Ely. The foundation stone of the Chapel was laid on the feast of St James, 25 July 1446, by the king; it was the first step in his plan for a great court, of which the Chapel was to form the north side.
Due to the Coronavirus outbreak and subsequent temporary closure of the private hospitals for consultations, I am offering private telephone consultations in place of face to face consultations.
Contact & Privacy Policy
Privacy Policy
Dr S J Middleton
PATIENT PRIVACY NOTICE
Note this policy is a continuation of that used when Dr Middleton was undertaking clinical work and therefore aspects of this policy are not relevant to his current medico-legal role.
As a clinician and therefore custodian of personal information , I must only use that information in accordance with all applicable law and guidance. This Privacy Notice provides you with a detailed overview of how I will manage your data from the point at which it is gathered and onwards, and how that complies with the law. I will use your personal information for a variety of purposes including, but not limited to, providing you with care and treatment, sharing it with other medical professionals and research/clinical audit programmes.
In addition, you have a number of rights as a data subject. You can, for instance, seek access to your medical information, object to me using your information in particular ways, request rectification of any information which is inaccurate or deletion of information which is no longer required (subject to certain exceptions). This Privacy Notice also sets out your rights in respect of your personal information, and how to exercise them.
For ease of reference, this Notice is broken into separate sections below with headings which will help you to navigate through the document. Introduction
This Privacy Notice sets out details of the information that I, as a clinician responsible for your treatment (and including my medical secretaries), may collect from you and how that information may be used. Please take your time to read this Privacy Notice carefully.
About me
In this Privacy Notice I use "I" or "mine" or "my" to refer to me as the clinician who is using your personal information.
In the event that you have any queries, comments or concerns in respect of the manner in which I have used, or potentially will use, your personal information then you should contact me directly and I would be happy to discuss further. Dr Stephen Middleton, 14 Meadow Road, Greatgransden, Bedfordshire, SG193BD.
Your personal data
I am a Data Controller in respect of your personal information which I hold about you. This will mainly relate to your medical treatment, but will be likely to also include other information such as financial data in relation to billing. I must comply with the data protection legislation and relevant guidance when handling your personal information, and so must any medical secretary who assists me in an administrative capacity. Your personal data may include any images taken in relation to your treatment which must not only be managed in accordance with the law, this Privacy Notice but also all applicable professional standards including guidance from the General Medical Council and British Medical Association.
I will provide your treatment from an independent private hospital and, in due course, it may be necessary for the independent private hospital to also process your personal data. I will do so in accordance with the law, the principles of this Privacy Notice and to the extent that it is necessary to do so. This could be where [Spire/other independent provider] needs to arrange other healthcare services as part of your treatment, such as nursing or dietician advice, or support other aspects of the treatment which I provide to you. In that case, the independent private hospital will become a joint Data Controller in respect of your personal information and you will be provided with a copy of their Privacy Notice which sets out how they will manage that information.
Your personal information will be handled in accordance with the principles set out within this Privacy Notice. This means that whenever I use your personal data, I will only do so as set out in this Privacy Notice. From time to time, I may process your personal information at a non- independent private hospital site (medical or non-medical), as may my medical secretary.
What personal information do I collect and use from patients?
I will use “special categories of personal information” (previously known as "sensitive personal data") about you, such as information relating to your physical and mental health.
If you provide personal information to me about other individuals (including medical or financial information) you should inform the individual about the contents of this Privacy Notice. I will also process such information in accordance with this Privacy Notice.
In addition, you should note that in the event you amend data which I already hold about you (for instance by amending a pre-populated form) then I will update our systems to reflect the amendments. Our systems will continue to store historical data.
Personal information
As one of my patients, the personal information I hold about you may include the following:
Name Contact details, such as postal address, email address and telephone number (including mobile number) Financial information, such as credit card details used to pay us and insurance policy details Occupation Emergency contact details, including next of kin Background referral details
Special Categories Personal Information
As one of my patients, I will hold information relating to your medical treatment which is known as a special category of personal data under the law, meaning that it must be handled even more sensitively. This may include the following:
Details of your current or former physical or mental health, including information about any healthcare you have received from other healthcare providers such as GPs, dentists or hospitals (private and/or NHS), which may include details of clinic and hospital visits, as well as medicines administered. I will provide further details below on the manner in which I handle such information. Details of services you have received from me Details of your nationality, race and/or ethnicity Details of your religion Details of any genetic data or biometric data relating to you Data concerning your sex life and/or sexual orientation
The confidentiality of your medical information is important to me, and I make every effort to prevent unauthorised access to and use of information relating to your current or former physical and mental health (or indeed any of your personal information more generally). In doing so, I will comply with UK data protection law, including the Data Protection Act 2018 and all applicable medical confidentiality guidelines issued by professional bodies including, but not limited to, the General Medical Council and the Nursing and Midwifery Council.
From 25 May 2018, the current Data Protection Act will be replaced by the EU General Data Protection Regulation (GDPR) and a new Data Protection Act. All uses of your information will comply with the GDPR and the new Data Protection Act from that date onwards
How do I collect your information?
I may collect personal information from a number of different sources including, but not limited to:
GPs Dentists Other hospitals, both NHS and private (including Spire/other independent provider) Mental health providers Commissioners of healthcare services Other clinicians (including their medical secretaries)
Directly from you
Information may be collected directly from you when:
You enter into a contract with me or independent private hospital for the provision of healthcare services You use those services You complete enquiry forms on the independent private hospital website You submit a query to me including by letter and email You correspond with me by letter, email, telephone incoming and outgoing calls from/to patients may be recorded.
From other healthcare organisations
My patients will usually receive healthcare from other organisations, and so in order to provide you with the best treatment possible I may have to collect personal information about you from them. These may include:
Medical records from your GP Medical records from other clinicians (including their medical secretaries) Medical records from your dentist Medical records from the NHS or any private healthcare organisation
Medical records include information about your diagnosis, clinic and hospital visits and medicines administered.
From third parties
As detailed in the previous section, it is often necessary to seek information from other healthcare organisations. I may also collect information about you from third parties when:
You are referred to me for the provision of services including healthcare services I liaise with your current or former employer, health professional or other treatment or benefit provider I liaise with your family I liaise with your insurance policy provider I deal with experts (including medical experts) and other service providers about services you have received or are receiving from me I deal with NHS health service bodies about services you have received or are receiving from us I liaise with credit reference agencies I liaise with debt collection agencies I liaise with Government agencies, including the Ministry of Defence, the Home Office and HMRC How will I communicate with you? I may communicate with you in a range of ways, including by telephone, SMS, email, and / or post. If I contact you using the telephone number(s) which you have provided (landline and/or mobile), and you are not available which results in the call being directed to a voicemail and/or answering service, I may leave a voice message on your voicemail and/or answering service as appropriate, and including only sufficient basic details to enable you to identify who the call is from, very limited detail as to the reason for the call and how to call me back.
However: to ensure that I provide you with timely updates and reminders in relation to your healthcare (including basic administration information and appointment information (including reminders)), I may communicate with you by SMS and/or unencrypted email (where you have provided me with your SMS or email address) [in each case where you have expressed a preference in the patient registration form to be contacted by SMS and / or email.]
to provide you with your medical information (including test results and other clinical updates) and/or invoicing information, I may communicate with you by email (which will be encrypted) where you have provided me with your email address and have expressed a preference in the patient registration form to be contacted by email. The first time I send you any important encrypted email that I am not also sending by post or which requires action to be taken, I will endeavour to contact you separately to ensure that you are able to access the encrypted email you are sent.
Please note that although providing your mobile number and email address and stating a preference to be communicated by a particular method will be taken as an affirmative confirmation that you are happy for us to contact you in that manner, I am not relying on your consent to process your personal data in order to correspond with you about your treatment. As set out further below, processing your personal data for those purposes is justified on the basis that it is necessary to provide you with healthcare service.
What are the purposes for which your information is used? I may 'process' your information for a number of different purposes, which is essentially the language used by the law to mean using your data. Each time I use your data I must have a legal justification to do so. The particular justification will depend on the purpose of the proposed use of your data. When the information that we process is classed as a “special category of personal information”, I must have a specific additional legal justification in order to use it as proposed.
Generally I will rely on the following legal justifications, or 'grounds': Taking steps at your request so that you can enter into a contract with me to receive healthcare services from us. For the purposes of providing you with healthcare pursuant to a contract between you and I. I will rely on this for activities such as supporting your medical treatment or care and other benefits, supporting your nurse, carer or other healthcare professional and providing other services to you. I have an appropriate business need to process your personal information and such business need does not cause harm to you. I will rely on this for activities such as quality assurance, maintaining my business records, monitoring outcomes and responding to any complaints. I have a legal or regulatory obligation to use such personal information. I need to use such personal information to establish, exercise or defend my legal rights. You have provided your consent to my use of your personal information. Note that failure to provide your information further to a contractual requirement with me may mean that I am unable to set you up as a patient or facilitate the provision of your healthcare.
I provide further detail on these grounds in the sections below.
Appropriate business needs
One legal ground for processing personal data is where I do so in pursuit of legitimate interests and those interests are not overridden by your privacy rights. Where I refer to use for my appropriate business needs, I am relying on this legal ground.
The right to object to other uses of your personal data
You have a range of rights in respect of your personal data, as set out in detail in this document. This includes the right to object to me using your personal information in a particular way (such as sharing that information with third parties), and I must stop using it in that way unless specific exceptions apply. This includes, for example, if it is necessary to defend a legal claim brought against me, or it is otherwise necessary for the purposes of your ongoing treatment.
You will find details of my legal grounds for each of our processing purposes below. I have set out individually those purposes for which I will use your personal information, and under each one I set out the legal justifications, or grounds, which allow me to do so. You will note that I have set out a legal ground, as well as an 'additional' legal ground for special categories of personal information. This is because I have to demonstrate additional legal grounds where using information which relates to a person's healthcare, as I will be the majority of the times I use your personal information.
Purpose 1: To set you up as my patient, including carrying out fraud, credit, anti-money laundering and other regulatory checks
Legal ground: Taking the necessary steps so that you can enter into a contract with me for the delivery of healthcare.
Additional legal ground for special categories of personal information: The use is necessary for reasons of substantial public interest, and it is also in my legitimate interests to do so.
Purpose 2: To provide you with healthcare and related services
Clearly, the reason you come to me is to provide you with healthcare, and so I have to use your personal information for that purpose.
Legal grounds: Providing you with healthcare and related services Fulfilling my contract with you for the delivery of healthcare
Additional legal grounds for special categories of personal information: I need to use the data in order to provide healthcare services to you The use is necessary to protect your vital interests where you are physically or legally incapable of giving consent
Purpose 3: For account settlement purposes
I will use your personal information in order to ensure that your account and billing is fully accurate and up-to-date
Legal grounds: My providing you healthcare and other related services Fulfilling my contract with you for the delivery of healthcare My having an appropriate business need to use your information which does not overly prejudice you
Your consent
Additional legal grounds for special categories of personal information: I need to use the data in order to provide healthcare services to you The use is necessary in order for me to establish, exercise or defend my legal rights Your consent
Purpose 4: For medical audit/research purposes
Clinical audit
Medical research
Legal grounds: I have a legitimate interest in helping with medical research and have put appropriate safeguards in place to protect your privacy
Additional legal grounds for special categories of personal information: The processing is necessary in the public interest for statistical and scientific research purposes
Purpose 5: Communicating with you and resolving any queries or complaints that you might have.
From time to time, patients may raise queries, or even complaints, with me and [Spire/other independent provider] and I take those communications very seriously. It is important that I am able to resolve such matters fully and properly and so I, as well as [Spire/other independent provider] will need to use your personal information in order to do so.
Legal grounds: Providing you with healthcare and other related services Having an appropriate business need to use your information which does not overly prejudice you
Additional legal grounds for special categories of personal information: The use is necessary for the provision of healthcare or treatment pursuant to a contract with a health professional The use is necessary in order for me to establish, exercise or defend my legal rights
Purpose 6: Communicating with any other individual that you ask us to update about your care and updating other healthcare professionals about your care.
Legal grounds:
Additional legal ground for special categories of personal information: I need to use the data in order to provide healthcare services to you The use is necessary for reasons of substantial public interest under UK law The use is necessary in order for me to establish, exercise or defend my legal rights
I also participate in initiatives to monitor safety and quality, helping to ensure that patients are getting the best possible outcomes from their treatment and care. The Competition and Markets Authority Private Healthcare Market Investigation Order 2014 established the Private Healthcare Information Network (“PHIN”), as an organisation who will monitor outcomes of patients who receive private treatment. Under Article 21 of that Order, I am required to provide PHIN with information related to your treatment, including your NHS Number in England and Wales, CHI Number in Scotland or Health and Care Number in Northern Ireland), the nature of your procedure, whether there were any complications such as infection or the need for readmission/admission to a NHS facility and also the feedback you provided as part of any PROMs surveys. PHIN will use your information in order to share it with the NHS, and track whether you have received any follow-up treatment. I will only share this information with PHIN if you have provided your consent for me to do so.
The records that I share may contain personal and medical information about patients, including you. PHIN, like me, will apply the highest standards of confidentiality to personal information in accordance with data protection laws and the duty of confidentiality. Any information that is published by PHIN will always be in anonymised statistical form and will not be shared or analysed for any purpose other than those stated. Further information about how PHIN uses information, including its Privacy Notice, is available at www.phin.org.uk. Purpose 7: Complying with our legal or regulatory obligations, and defending or exercising our legal rights
Legal grounds:
Additional legal ground for special categories of personal information: I need to use the data in order for others to provide informed healthcare services to you The use is necessary for reasons of the provision of health or social care or treatment or the management of health or social care systems
The use is necessary for establishing, exercising or defending legal claims
Purpose 8: Managing my business operations such as maintaining accounting records, analysis of financial results, internal audit requirements, receiving professional advice (e.g. tax or legal advice)
In order to do this, I will not need to use your special categories of personal information and so I have not identified the additional ground to use your information for this purpose.
Legal grounds: My having an appropriate business need to use your information which does not overly prejudice you
Purpose 9: Provide marketing information to you (including information about other products and services offered by selected third-party partners) in accordance with preferences you have expressed.
Legal grounds: My having an appropriate business need to use your information which does not overly prejudice you
You have provided your consent
Disclosures to third parties:
I may disclose your information to the third parties listed below for the purposes described in this Privacy Notice. This might include:
A doctor, nurse, carer or any other healthcare professional involved in your treatment Other members of support staff involved in the delivery of your care, like receptionists and porters Anyone that you ask me to communicate with or provide as an emergency contact, for example your next of kin or carer NHS organisations, including NHS Resolution, NHS England, Department of Health Other private sector healthcare providers Your GP Your dentist Other clinicians (including their medical secretaries) Third parties who assist in the administration of your healthcare, such as insurance companies Private Healthcare Information Network National and other professional research/audit programmes and registries, as detailed under purpose 4 above Government bodies, including the Ministry of Defence, the Home Office and HMRC Our regulators, like the Care Quality Commission, Health Inspectorate Wales and Healthcare Improvement Scotland The police and other third parties where reasonably necessary for the prevention or detection of crime Our insurers Debt collection agencies Credit referencing agencies Our third party services providers such as IT suppliers, actuaries, auditors, lawyers, marketing agencies, document management providers and tax advisers aSelected third parties in connection with any sale, transfer or disposal of our business I may also use your personal information to provide you with information about products or services which may be of interest to you where you have provided your consent for me to do so.
I may communicate with these third parties in a variety of ways including, but not limited to, email, post, fax and telephone.
What marketing activities do I carry out?
I may also use your personal information to provide you with information about products or services which may be of interest to you where you have provided your consent for me to do so.
If you receive any marketing communications and you no longer wish to receive these , you can click on the "unsubscribe" link that appears in these emails, otherwise you can always contact me using the details set out in section 3 to update your contact preferences.
If you do not wish to receive non-website based marketing information, please contact me.
Automated Decision Making
An automated decision is a decision made by computer without any human input, and there will be no automated decision-making in relation to your treatment or other decisions which will produce legal or similarly significant effects.
How long do I keep personal information for?
I will only keep your personal information for as long as reasonably necessary to fulfil the relevant purposes set out in this Privacy Notice and in order to comply with my legal and regulatory obligations.
If you would like further information regarding the periods for which your personal information will be stored, please contact me using the details outlined in section 3.
International data transfers
I (or third parties acting on my behalf) may store or process information that we collect about you in countries outside the European Economic Area ("EEA"). Where I make a transfer of your personal information outside of the EEA I will take the required steps to ensure that your personal information is protected.
I have no current practice of transferring data outside the EEA and if this becomes required as part of your health care it will only be undertaken with your explicit permission such as when contacting another medical / healthcare working who is involved in your healthcare and requires information from myself.
If you would like further information regarding the steps I take to safeguard your personal information, please contact me using the details provided in section 3 above.
Please note that we have listed above the current common transfers of personal data outside of the EEA but it may be necessary, in future, to transfer such data for other purposes. In the event that it is necessary to do so, we will update this Privacy Notice.
Your rights
Under data protection law you have certain rights in relation to the personal information that I hold about you. These include rights to know what information I hold about you and how it is used. You may exercise these rights at any time by contacting me using the details provided at section 3 above.
There will not usually be a charge for handling a request to exercise your rights.
If I cannot comply with your request to exercise your rights we will usually tell you why.
There are some special rules about how these rights apply to health information as set out in legislation including the Data Protection Act (current and future), the General Data Protection Regulation as well as any secondary legislation which regulates the use of personal information.
If you make a large number of requests or it is clear that it is not reasonable for me to comply with a request then we do not have to respond. Alternatively, I can charge for responding.
Your rights include:
The right to access your personal information
You are usually entitled to a copy of the personal information I hold about you and details about how I use it.
Your information will usually be provided to you in writing, unless otherwise requested. If you have made the request electronically (e.g. by email) the information will be provided to you by electronic means where possible.
Please note that in some cases I may not be able to fully comply with your request, for example if your request involves the personal data of another person and it would not be fair to that person to provide it to you.
You are entitled to the following under data protection law. Under Article 15(1) of the GDPR I must usually confirm whether I have personal information about you. If I do hold personal information about you I usually need to explain to you: The purposes for which I use your personal information The types of personal information I hold about you Who your personal information has been or will be shared with, including in particular organisations based outside the EEA. If your personal information leaves the EU, how I will make sure that it is protected Where possible, the length of time I expect to hold your personal information. If that is not possible, the criteria I use to determine how long I hold your information for If the personal data I hold about you was not provided by you, details of the source of the information Whether I make any decisions about you solely by computer and if so details of how those decision are made and the impact they may have on you Your right to ask me to amend or delete your personal information Your right to ask me to restrict how your personal information is used or to object to my use of your personal information Your right to complain to the Information Commissioner's Office
I also need to provide you with a copy of your personal data, provided specific exceptions and exemptions do not apply.
The right to rectification
I take reasonable steps to ensure that the information I hold about you is accurate and complete. However, if you do not believe this is the case, you can ask me to update or amend it.
The right to erasure (also known as the right to be forgotten)
I may update this Privacy Notice from time to time to ensure that it remains accurate, and the most up-to-date version can always be found at my practice address. In the event that there are any material changes to the manner in which your personal information is to be used then I will provide you with an updated copy of this Privacy Notice.
In some circumstances, you have the right to request that I delete the personal information I hold about you. However, there are exceptions to this right and in certain circumstances I can refuse to delete the information in question. In particular, for example, I do not have to comply with your request if it is necessary to keep your information in order to perform tasks which are in the public interest, including public health, or for the purposes of establishing, exercising or defending legal claims.
The right to restriction of processing
In some circumstances, I must "pause" our use of your personal data if you ask me to do so, although I do not have to comply with all requests to restrict my use of your personal information. In particular, for example, I do not have to comply with your request if it is necessary to keep your information in order to perform tasks which are in the public interest, including public health, or for the purposes of establishing, exercise or defending legal claims.
The right to data portability
In some circumstances, I must transfer personal information that you have provided to you or (if this is technically feasible) another individual/ organisation of your choice. The information must be transferred in an electronic format.
The right to object to marketing
The right to withdraw consent In some cases I may need your consent in order for my use of your personal information to comply with data protection legislation. Where we do this, you have the right to withdraw your consent to further use of your personal information. You can do this by contacting me using the details provided at section 3 above.
The right to complain to the Information Commissioner's Office
You can complain to the Information Commissioner's Office if you are unhappy with the way that I have dealt with a request from you to exercise any of these rights, or if you think I have not complied with our legal obligations.
More information can be found on the Information Commissioner’s Office website: https://ico.org.uk/
Making a complaint will not affect any other legal rights or remedies that you have.
National Data Opt-Out Programme
NHS Digital is currently developing a national programme which will go live on 25 May 2018, pursuant to which all patients will be able to log their preferences as to sharing of their personal information. All health and care organisations will be required to uphold patient choices, but only from March 2020. In the meantime you should make me aware directly of any uses of your data to which you object.
Updates to this Privacy Notice
I may update this Privacy Notice from time to time to ensure that it remains accurate. In the event that these changes result in any material difference to the manner in which I process your personal data then I will provide you with an updated copy of the Policy.
This Privacy Notice was last updated on the 27/11/2023.